The Big C
Prologue: The sound, the fear and the fury
Until roughly 50 years ago, just saying the word “cancer” aloud was something akin to a cursed incantation, archived only in medical textbooks and obituaries out of fear of lending it the power of speech.
Because the treatment options available before that time did little to considerably lengthen or improve the lives of those with cancer, speaking its name was considered an invitation for death itself, a sentence passed by a chaotic, unknowable force that claimed the lives of loved ones without warning. The “Big C” was only alluded to in urgent whispers so as to keep the disease at bay.
Former National Cancer Institute Director Vincent T. DeVita Jr., M.D., notes this cultural avoidance during the 1940s as he recalls his aunt’s ovarian cancer diagnosis in his 2015 book, “The Death of Cancer.”
“It was such a dreadful diagnosis, in fact, that many people, including my parents, couldn’t bring themselves to utter the word. If they did, it was in a whisper – ‘cancer’ – as if there were something shameful about it,” he writes. “Or maybe it was superstition, the fear that merely saying the word out loud was tempting fate, like waving a red cape in front of a bull.”
Otis Brawley, M.D., former assistant director at the NCI and globally recognized expert in cancer prevention and control, has also noted that this collective anxiety around the word “cancer” continued into the second half of the 20th century.
“Even when I was a kid in the 1960s, people would call it the ‘Big C’ and whisper it,” Brawley told U.S. News & World Report in 2018.
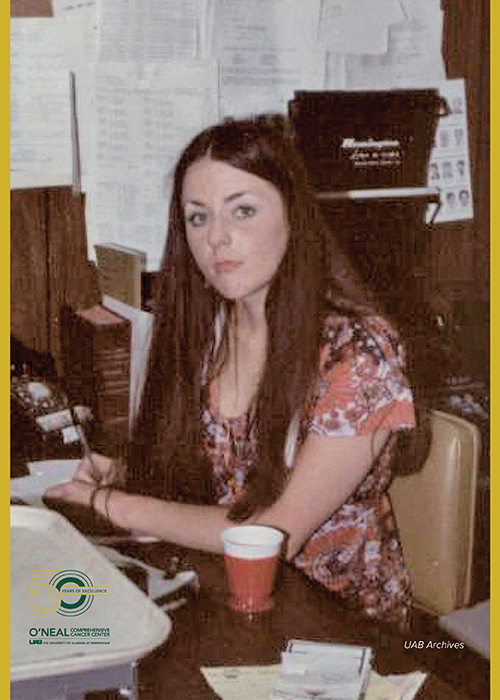
Joan Kemp, longtime assistant to the director of what would later become the UAB O’Neal Comprehensive Cancer Center, says she remembers a fear that seemed to grip the public consciousness in the decades leading up to the National Cancer Act of 1971 and the founding of the O’Neal Cancer Center.
“Some people felt like, if they didn’t talk about it, it didn’t exist – that kind of thing,” she said. “But I think it was just the fear or the reality that, in the past, cancer had been such a deadly disease.”
Even those with the means to seek and obtain treatment from a specialty cancer hospital or clinic at the time were not guaranteed to live significantly longer after a diagnosis than those who were unable to get the same kind of specialized cancer care.
“People didn’t want to talk about it because it just seemed that, if you had cancer, you just died,” Kemp said. “And more or less, in the 60s and early 70s and before, that’s what happened. You got cancer, and you died.”
Kemp served as assistant to the director of the Cancer Center years before there was ever a center to direct. She was there alongside John Durant, M.D., who was initially recruited to the UAB School of Medicine in 1968 by its then-dean, S. Richardson Hill Jr., M.D., to serve as cancer planning coordinator. Kemp was there when the cancer program was first formalized at UAB, when Durant became its director in 1970 and when it became an NCI-Designated Cancer Center roughly two years later.
Kemp was at the Cancer Center for nearly 50 years, from the early days of many cancer treatments when options were still scarce, until she retired in 2017.
“Now, a lot of people during their treatments, they just go on about their normal, daily routines and, more or less, get through it, whereas, in the past, that’s not what happened,” she said.
In Bruce L. Patterson’s 1996 book, “A Legacy of Love: The Story of the Lurleen B. Wallace Foundation and the Courage Crusade,” Kemp, Durant, Hill and other pioneers of the O’Neal Cancer Center and UAB recount the years before the founding of the Cancer Center, as well as the fearful uneasiness that shrouded the topic of cancer.
“If you look back in history, you’ll find that cancer was usually a taboo subject,” Hill is quoted as saying. “It was not something you talked about in polite company.”
The best cancer care in the country at the time was out of state and still only comprised treatments that some members of the public believed to be just as lethal as the cancer. But following the cancer diagnosis and death of former Alabama Governor Lurleen Wallace in 1968, the statewide push to establish Alabama’s first and only specialized cancer treatment facility was more than a desire to bring that care home. For many, it was a collective rage against a disease whose name they dared not even speak.
“In the 1960s, there were still sensitivities, not only about cancer but particularly about cervical cancer,” Hill continues. Although Wallace was initially diagnosed with uterine cancer, the specificity of her diagnosis was not then public knowledge. “I didn’t realize it at the time, but the newspapers then referred to Governor Lurleen’s cancer only as ‘abdominal cancer.’”
The grassroots campaign for an in-state cancer hospital became a battle cry for everyone who had lost someone they loved to cancer, from the rich and powerful to the poor and marginalized.
In the years that passed, the cancer program that was established in the iron-red soil of the city of Birmingham gave rise to the infrastructure of the UAB O’Neal Comprehensive Cancer Center.
Scientists, doctors and supporters from across the Deep South, the United States and the world saw the potential to change the structural landscape and cultural conversation surrounding cancer care and cancer research at UAB by building anew in the Magic City.
“It’s been amazing to me, over the years, to see patients with the same kind of disease that would have then been, more or less, a death sentence, and to then see that – a few years later – they could be treated and be back at work in their normal lives,” Kemp said. “But it took a lot of hard work, a lot of funding from various sources, a lot of people working really hard at different levels to achieve that.”
Part I: Surgical Oncology
While the clinical and cultural reality of cancer for the people of Alabama did not change overnight, the staples of cancer treatment were beginning to evolve, starting with the practice of what has since become the field of surgical oncology.
Marshall Urist, M.D., professor emeritus in the UAB Department of Surgery and senior scientist at the O’Neal Cancer Center, reflects on tales from the early days of the Cancer Center when cancer was not so deeply embedded within the public consciousness.
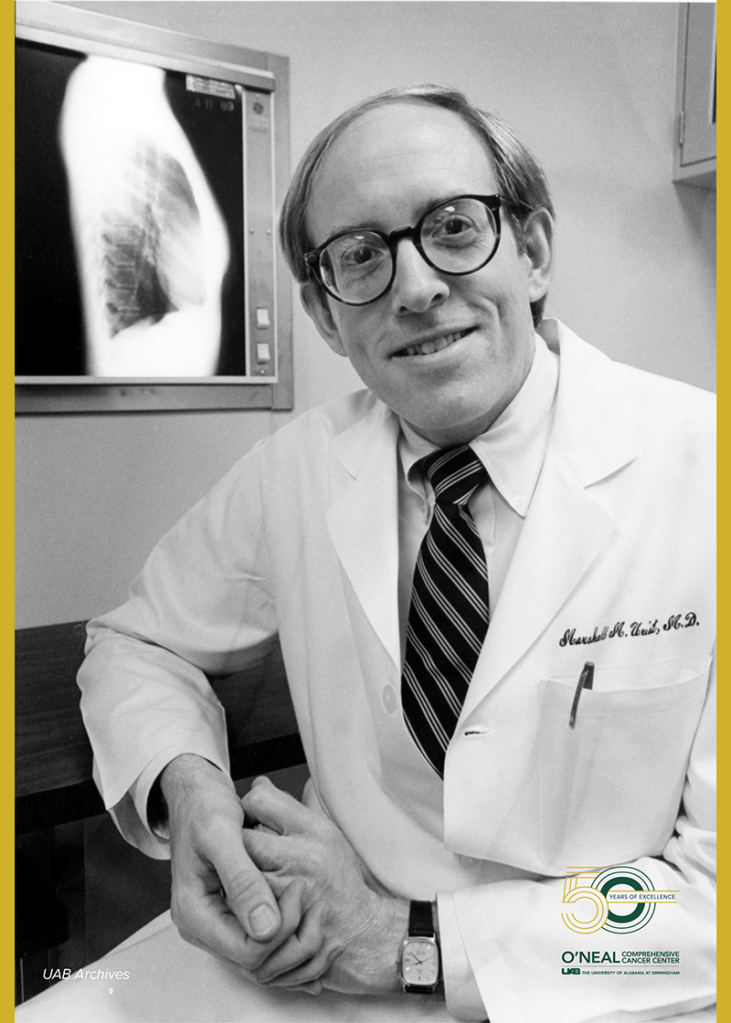
“Everyone has heard the stories about patients, families and doctors who would not use the word ‘cancer’ because it would make the patient give up hope,” he said. “But that was not uncommon at that time.”
Urist cites the development and proliferation of anesthesia as one of the first major turning points in the evolution of surgery.
“Surgery’s role in the treatment of cancer dates back to ancient civilizations and the excision of surface growths,” Urist said. “The development and refinement of anesthesia enabled the safe resection of larger and internal tumors. With time, it became clear which patients could have smaller operations and who benefited from larger resections.”
Fellow Professor Emeritus and O’Neal Cancer Center Senior Scientist Kirby Bland, M.D., is another veteran of the Cancer Center and of surgical oncology at UAB. Bland was recruited more than 20 years ago to serve as the chair of the UAB Department of Surgery from 1999 to 2015. Soon after his recruitment, Bland was also appointed the deputy director of the Cancer Center, where he served for 10 years under the leadership of former O’Neal Cancer Center directors Albert LoBuglio, M.D., and Edward Partridge, M.D. Bland now continues to serve as a senior advisor to the current director of the O’Neal Comprehensive Cancer Center, Barry Sleckman, M.D., Ph.D.
“Surgery has been a principal discipline – and prominently remains a major modality in this era – for the management of cancer of various organ sites over thousands of years,” Bland said. “Although the biology of cellular dedifferentiation and the kinetics for tumor growth would not be forthcoming for centuries in the diagnosis and treatment of cancer for many solid tumor variants, measures for surgical removal of the cancerous growth would become the principal modality utilized in the management of all tumors.”
Bland says that, although surgery has been a part of cancer therapies for centuries, it has grown into a robust, multidisciplinary field as surgeons and scientists have come to better understand cancer biology, pathology and physiology alongside other similarly growing specialties that have only developed over the past 50 to 100 years.
“While surgery has been in use for the therapy of cancers for hundreds of years, only the advancements of the 20th and 21st centuries have provided major impact for localized recurrence and survival with adjuvant therapies,” Bland said. “These adjuvant therapies now include advanced targeted radiotherapy; medical oncology therapy with cytotoxic agents in hormonal-positivity (anti-hormonals); and receptor biology to direct cellular and nucleolus-focused monoclonal antibody binding, which have been assisted by evolving advancements of molecular medicine.”
Clinical trials, combination treatments and staging
Soon after the Cancer Center was established, surgeons and medical oncologists across Alabama participated in a groundbreaking clinical trial centered at UAB to compare the results of two surgical techniques used to treat breast cancer: the modified radical mastectomy and the standard radical mastectomy.
This prospective randomized trial was conducted by the UAB Department of Surgery’s chief of surgical oncology at the time, William Maddox, M.D., and other Cancer Center faculty as part of the Alabama Breast Cancer Project. The study concluded that the outcomes of the two techniques were equivalent, meaning that there was no significant benefit to performing a more debilitating resection.
“It is interesting that we had already begun to perform even smaller procedures, such as lumpectomy, by the time the results of the Alabama Breast Project were published,” Urist said.
In the early 1980s, the U.S. Department of Veterans Affairs also conducted an important clinical trial in which participating hospitals were randomized such that patients with advanced larynx cancer would receive either surgery as their initial treatment or chemotherapy and radiation as their initial treatment.
“I think that was one of the earliest randomized clinical trials done through the Cancer Center, at least where surgical trials are concerned,” Urist said.
At the time, surgery was still considered by most to be the best first-line treatment for locally advanced larynx cancers, but it was a complicated procedure that often left patients with long-term difficulty swallowing or with the loss of their natural voice. The results of the trial, published in the New England Journal of Medicine in 1991, reported that some patients who received chemotherapy and radiation first responded well to that treatment combination and did not require the surgery.
“The trial showed that some patients could avoid an operation by starting with chemotherapy and radiation,” Urist said. “So UAB had a great interest in exploring the appropriate role of surgery in the treatment of cancer patients from the time of the origin of the Cancer Center.”
In addition to reducing the need for unnecessary, larger-scale operations, surgeons and scientists were finding new, more effective methods for biopsy and staging. According to the National Cancer Institute, a staging system is a method of cancer classification that is used to evaluate the extent of cancer within the body, usually through physical exams, imaging tests and biopsies of affected areas.
The surgical stage, or pathologic stage, of a particular cancer is determined by examining tissue that is removed during an operation. These developments in staging allowed surgeons, pathologists and other clinicians or scientists to learn how cancer spreads throughout the body and to determine which patients were most likely to benefit from a surgery, as well as at what point in time that surgery was expected to have the greatest impact on their cancer.
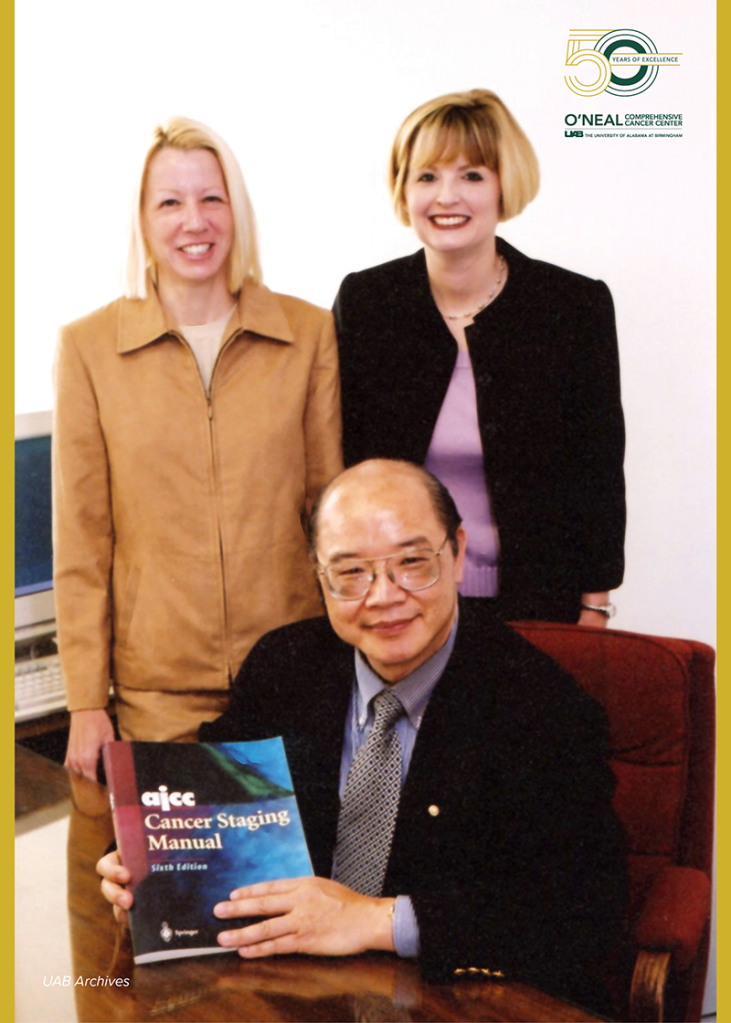
In 1975, a team of Cancer Center investigators led by Charles Balch, M.D., former director of surgical oncology at UAB, laid the foundation for advancements in staging when they created a special research program and database to study melanoma, the deadliest kind of skin cancer. In conjunction with the University of Sydney in Australia, the project provided a multifactorial analysis of survival results to enable surgeons to choose the most effective treatment option for melanoma patients.
In addition to Balch, the team also included several other key players at UAB who held leadership positions at the time, including Maddox, who was still serving as the chief of surgical oncology; Seng-jaw Soong, Ph.D., the director of the Cancer Center’s Biostatistics Unit; Tarig Murad, M.D., the chief of surgical pathology; and, later, Urist, who joined the team soon after arriving at UAB in 1981 and who became chief of surgical oncology in 1985.
Over the next decade or two, this team of UAB cancer faculty used its comprehensive database, a series of robust studies and a variety of powerful mathematical and statistical tools to gain some valuable insights on melanoma. Then, in 2001, the Cancer Center’s Biostatistics Unit led a statistical study that became the basis for a new cutaneous melanoma staging system for the American Joint Committee on Cancer. The new staging system, which went into effect in 2002, was the sixth revision of the AJCC’s guidelines for evaluating melanoma and was developed through a collaboration between UAB and an international team of major melanoma centers and study groups across the globe.
Additionally, as pathology-based diagnostic techniques and imaging techniques, such as CT scans, MRIs and PET scans, improved, surgeons were better able to use staging to predict how patients and their tumors would respond to different kinds of treatment.
“With the advent of CT scans, MRIs and, now, PET scans, we could stage patients much more accurately,” Urist said. “Over many years, we have learned how to combine the benefits of surgery, chemotherapy and radiation therapy to achieve the best results for each patient.”
Laparoscopic and robotic surgery
The development of minimally invasive surgery, in which a tiny camera and light are inserted into the body through one or more small incisions, allowed surgeons to improve patients’ post-operative recovery by reducing their pain, while avoiding unnecessary risk to healthy tissue.
“From a surgical point of view, of course, the first thing was laparoscopic surgery,” Urist said. “And as that became more advanced, then there were resection techniques that are purely laparoscopic, and then there are ones that combined hand-assisted or partially laparoscopic procedures, all to enhance post-operative recovery.”
Once robot-assisted laparoscopic surgery came to UAB with the introduction of Intuitive’s da Vinci system in 2004, surgeons were able to view the inside of a patient’s body in three dimensions, allowing them to perform operations with more precision. Robotic surgery is another form of minimally invasive surgery that uses small, wristed instruments on robotic arms controlled by a surgeon through an intuitive computer console system.
John Porterfield, M.D., is a professor in the UAB Department of Surgery and former director of the UAB General Surgery Residency Program. Over his 14 years at UAB, Porterfield has worked with every UAB department that uses the surgical robot and, as a result, helped integrate robotic surgery training within the curriculum for general surgery residents.
“The stability and capability of the three-dimensional view from the robotic camera changed minimally invasive surgery permanently,” Porterfield said. “This allows us to operate with more precision, tremor control and other advanced technologies that give us the opportunity to push far beyond the limits of laparoscopy.”
By 2008, the Cancer Center had become the first medical center in Alabama and one of the first in the United States to offer da Vinci robotic surgery as a treatment for head and neck cancer and bladder cancer, as well as one of the first institutions in Alabama to offer this robotic surgery to prostate cancer patients. Since then, UAB’s robotic surgery program has become one of the largest of its kind in the Southeast and now offers robotic surgery for each FDA-approved area served by UAB Medicine.
UAB has also acquired other robotic surgery systems that have further improved patient outcomes and reduced recovery time. One such system, added in 2019, is the da Vinci SP Single Port Surgical System, which enables surgeons to enter the body through one small incision, just longer than 1 inch, in the abdomen before deploying the robot’s flexible surgical instruments.
“One of the biggest things that differentiates us from other centers is that, for some select patients, we can safely perform outpatient single-port prostatectomies and other advanced procedures, so those patients don’t have to stay overnight in the hospital,” Porterfield said.
This technology is especially useful in treating urologic and oropharyngeal cancers because it allows surgeons to access more narrow spaces with improved visualization and precision.
“To be able to see individual nerves and to dissect along planes with a robot has greatly facilitated – and required that technology for – that advancement,” Urist said. “With a robot, you can do things that you can’t begin to do with human hands. You can do it in a smaller space and at different angles and have a view that you wouldn’t be able to get any other way. So it’s a great advancement in treatment.”
Knowledge is power
The field of surgical oncology has changed significantly over the past 50 years as technology has developed and cancer care has become more interdisciplinary.
“To begin with, the patient is a different person now than then, because cancer is not the taboo subject that was so commonly the case at that time,” Urist said. “They’re much more aware of the fact that there are other treatments, besides surgery, for cancer and that they can expect to be treated by a team of people and not just the doctors, no matter what type of treatment they’re receiving.”

When looking to the future of surgical oncology at UAB, Bland and Urist also reflect on the past. The comprehensive, multidisciplinary, translational approach to cancer care and cancer research that has come to define the O’Neal Cancer Center, they suggest, has been at the heart of surgical cancer care since the Cancer Center was first established.
“Each discipline has evolved into an array of robust specialties,” Bland said. “Contemporary medicine has evolved as clinicians, scientists and molecular biologists have long been engaged in protocols focused on translating targeted molecules or cellular receptors into complex, contemporary, therapeutic options, which span various broad disciplines of the oncology field, including surgery, radiation oncology, medical oncology, pathology, radiologic imaging, pharmacokinetics, genetics, stem cell transplantation, medical biostatistics and epidemiology to advance individual therapies for specific cancer variants.”
Over the past 50 years, this interdisciplinary approach may have also contributed to a cultural shift in the way patients, clinicians, researchers and administrators, as well as the public at large, tend to conceptualize cancer, at least in the state of Alabama.
“The difference is that, today, patients are much more familiar with the concept of cancer and the idea that the cancer treatment can lead to a cure,” Urist said. “And the other thing that’s changed is how many patients come with very good questions about their options for treatment.”
Urist also credits public health education for removing some of the stigma associated with cancer. This gave patients a more informed, active role in their care and demonstrated the need for that care to become more interdisciplinary.
“With time, with education, with the spread of all the information about the disease and the fact that it’s not a fatal diagnosis in so many cases, things began to change,” Urist said. “So public education played an enormous role in that process, but it was slow.”
An Alabama native and an established breast cancer surgeon, Bland is no stranger to the value of cancer education and awareness, especially among medically underserved and marginalized communities in the South. As deputy director of the O’Neal Cancer Center, Bland served alongside LoBuglio and a team of other UAB co-investigators on the O’Neal Cancer Center’s $13.8 million breast cancer Specialized Program of Research Excellence, or SPORE, grant from the NCI in 2000.
Coupled with UAB’s existing $9 million ovarian cancer SPORE, which was awarded in 1999 and for which Partridge served as principal investigator, the UAB O’Neal Comprehensive Cancer Center became the only academic institution in the country at the time to hold funded SPOREs in both ovarian cancer and breast cancer.
“Both SPOREs would focus on diseases that predominantly affected women and, of equal importance, possessed prevalent incidence within the minority and disparity populations of Alabama,” Bland said. “These observations were especially prevalent among Black women within the geographically designated Black Belt region of the United States, which extended from South Carolina through Georgia and Alabama to the Mississippi Delta and Arkansas.”
In 2007, the NCI awarded UAB its second breast cancer SPORE at $11.5 million, and over the next few years, awarded major extensions to the supplemental funding of other ongoing, noteworthy breast cancer projects at the Cancer Center, which provided a total of nearly $30 million in additional breast cancer SPORE funding over the 13-year funding cycle of these awards.
For decades, Bland, Partridge and a team of other SPORE investigators worked to reduce cancer incidence, morbidity and mortality for the people of Alabama most affected by breast cancer. This longstanding work, fortified by the breast cancer SPORE, ultimately led to the creation of the Deep South Network for Cancer Control, which became the basis of what is now the O’Neal Cancer Center’s Office of Community Outreach & Engagement.
“The most notable command of the O’Neal Comprehensive Cancer Center has been its work to increase education and awareness of cancer morbidity and mortality in the medically underserved populations of Alabama and its Black Belt,” Bland said. “I believe UAB and the O’Neal Cancer Center will become a long-recognized leader in community outreach and education.”
Part II: Radiation Oncology
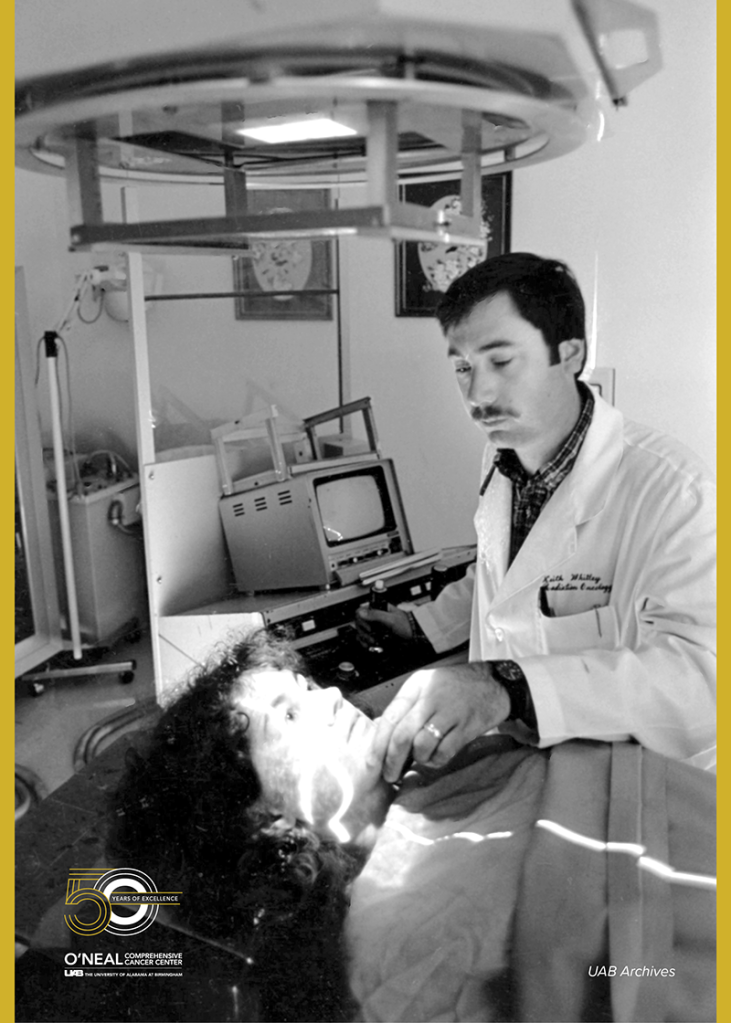
Fifty years ago, radiation therapy was a burgeoning field that had just begun to develop new methods of delivering radiation to cancers, especially those within deep tissues. Before the 1970s and 1980s saw the successful application of higher-energy beams in radiotherapy, patients who had cancer in the preceding two decades were commonly treated with lower-energy beams administered through a method called Cobalt teletherapy or with megavoltage X-rays made possible by the use of more advanced linear accelerators, also known as LINACs.
3D conformal and intensity-modulated radiation therapy
Further advancements in computer technology in this decade led to the widespread use of computer tomography, or CT, imaging, which was later used to develop three-dimensional conformal radiation therapy. This 3D conformal radiation therapy used CT imaging to map, or conform, static beams of radiation to the shape of a tumor inside the body using small sheets of lead, called collimators, to guide the beams.

Before CT imaging was widely used in radiation therapy, experts in radiographic imaging could only plan treatments in two dimensions, often by referencing cross-sectional images of a tumor and the anatomy of a treatment site.
However, the proliferation of CT imaging in the 1970s; the development of multi-leaf collimators, or MLCs, in the 1980s; and the rapid evolution of computers in the 1990s allowed 3D conformal radiation therapy and its contemporary, intensity-modulated radiation therapy, to become the standard for radiation delivery.
Like 3D conformal radiation therapy, intensity-modulated radiation therapy, or IMRT, uses CT scans to create three-dimensional images of a tumor site that inform the direction and angle of particle beams in radiation therapy. But with the addition of new forms of imaging such as magnetic resonance imaging, or MRI, as well as the integration of both fixed-beam MLCs and rotating-beam MLCs, IMRT became the most effective method for radiotherapy treatment. Since its development in the 1990s and 2000s, IMRT has also paved the way for new, more targeted methods of delivering multiple beams of radiation to a tumor, while reducing damage to the healthy tissue nearby.
Eddy Yang, M.D., Ph.D., is a co-leader of the Experimental Therapeutics Research Program at the UAB O’Neal Comprehensive Cancer Center, the deputy director and associate director for precision oncology at the Hugh Kaul Precision Medicine Institute at UAB, and the vice chair for translational science in the UAB Department of Radiation Oncology.
“And so that’s where the inverse planning of IMRT comes in,” Yang said. “You tell a computer how much of the dose you want to deliver and tell it how much you want to limit the normal tissue, and then it generates this algorithm that moves those MLCs accordingly to generate the dose that you wanted.”
As a cancer radiation specialist and a senior scientist at the O’Neal Cancer Center, Yang considers how the intrinsic goals of radiation therapy as a clinical practice have led to so many advancements in radiation delivery methods over the past 50 years.
“Ultimately, we want to better refine delivery of radiation to really target the areas of the cancer that need the higher doses due to its biology, while at the same time, reducing the radiation in areas that we don’t need it,” Yang said. “And that can help, in the long run, to optimize and personalize dose delivery to the tumor and spare normal tissue toxicity.”
Arc radiation therapy
In the late 2000s and early 2010s, one such method was the RapidArc system, manufactured by Varian Medical Systems, Inc. This system and its successors allowed multiple beams of radiation to be directed at a tumor from a variety of different angles as the beams themselves were attached to an arm that rotated around the patient, reducing the amount of time required for the patient to receive a particular dose of radiation.
In 2008, UAB became the first medical center in the United States to use the RapidArc system, which was revolutionary in that it could turn a 20-minute radiotherapy session into a 90-second radiotherapy session for many patients. This method used a system of powerful computers that could account for thousands of biological and mathematical variables, including scans of a patient’s tumor, to help doctors develop more informed strategies for a patient’s radiation treatments.
“When it comes to all those technological advances, we were right in the midst of being one of the first in the country or in the world to have those technologies here at UAB,” Yang said.
Nearly 10 years after the introduction of the RapidArc system, UAB also became the first medical center in the United States to use Varian’s newest volumetric modulated arc therapy system, called Varian HyperArc High-Definition Radiotherapy, for complex radiosurgical procedures in 2017. The HyperArc system, which Varian tested and partially developed in collaboration with UAB, was able to deliver more compact radiation doses that closely conformed to the size, shape and location of complex tumors, such as those present in brain cancer, while sparing more healthy tissue than what was possible to spare before.
Due to its high-definition MLCs and prescriptive capabilities, including patient immobilization, patient setup, imaging, simulation guidelines and predetermined delivery sequence, the HyperArc system removed the need to reposition a patient during a radiation therapy session, which allowed clinicians to irradiate multiple tumors simultaneously and to better manage patient movement and treatment planning.
Adaptive radiation therapy and proton therapy
Now, UAB has acquired the Varian Ethos system, which uses artificial intelligence and machine learning to adjust the target, angle, duration, dose and intensity of a patient’s radiotherapy treatment in real time based on current scans of a patient’s body. This method, referred to generally as adaptive radiation therapy, has been called radiation oncology’s contribution to personalized medicine.
“It’s about the ability to really shape that beam over the patient’s treatment course, taking into account the patient’s anatomy for each treatment,” Yang said.
The Ethos system at UAB is the first system of its kind in the world to combine the Ethos system with the Varian Identify Surface imaging system to better identify patients, position patients for treatment, set up system accessories and monitor patient motion throughout treatment without increasing the amount of radiation given to the patient.
“Ethos is another tool that helps aim radiation at the tumor target and avoid healthy tissue, much as proton therapy does,” said UAB Assistant Professor of Radiation Oncology Dennis Stanley, Ph.D., to UAB News when the system was first installed in August 2021. “This is a valuable option for patients who are not candidates for protons, or any of our other radiation delivery systems.”
In 2020, Proton International at UAB opened the state of Alabama’s first proton therapy center, the heart of which was a new cyclotron that would use Varian’s ProBeam proton therapy system to produce and deliver beams of radiation to treat patients with single-site tumors or, in some cases, metastatic tumors. The $25 million, 90-ton cyclotron, affectionately nicknamed Emma, is primarily used to administer this kind of proton therapy to cancer patients in a clinic staffed entirely by radiation oncologists, medical physicists, dosimetrists, radiation therapy technologists and nurses from the O’Neal Comprehensive Cancer Center and UAB.
Combination radiation therapies
In recent years, research has also shown that certain combinations of radiation therapy, surgery, chemotherapy and immunotherapy can lead to significantly better outcomes for many cancer patients.
One of the most important developments in this area was the discovery that combining radiation therapy with the drug cetuximab, or Erbitux, could reduce mortality without increasing the toxic effects of radiation therapy for patients with head and neck cancer.
The results of the trial, led by Department of Radiation Oncology Chair James Bonner, M.D., and published in the New England Journal of Medicine in 2006, suggested that cetuximab could improve locoregional control, increase the damage to cancer cells targeted by radiation therapy and avoid the toxic effects of radiotherapy to the head and neck. Cetuximab is a monoclonal antibody that inhibits the epidermal growth factor receptor that contributes to cancer cell proliferation.
“That trial showed that antibodies, plus radiation, could shrink tumors,” said former director of the O’Neal Cancer Center, Albert LoBuglio, M.D., to UAB News in 2017. “We published that and then went in and did pivotal trials for FDA approval of the drug, which became Erbitux.”
LoBuglio was director of the Cancer Center from 1983 to 2004 and worked closely with Bonner and others to study monoclonal antibodies.
“That’s still one of the primary treatments for head and neck cancer, and the pivotal trial was done here with our chair of radiation therapy as the principal investigator,” LoBuglio said.
Since then, researchers have found that the doses of radiation given to some stereotactic radiosurgery patients can also stimulate the immune system and could potentially augment a patient’s response to immunotherapy.
“As the research continued and we were figuring out better ways to deliver radiation, we also investigated novel agents that we can combine with radiation to make it work better, with the goal to advance the treatment options for patients and potentially improve outcomes through clinical trials,” Yang said. “We’re now figuring out the synergies of radiation with other targeted therapies and immunotherapies.”
In 2013, UAB installed its first cyclotron in the basement of the Wallace Tumor Institute, the home of the O’Neal Comprehensive Cancer Center. A cyclotron is a particle accelerator that collides protons with a target to create radioactive medical imaging agents that can be used in research or to diagnose or treat patients. At the time, the 61,000-pound TR24 cyclotron was the most powerful cyclotron at any academic medical center in the United States. It opened the door for many new applications in cancer care and cancer research.
Over the past decade, this cyclotron, in addition to the O’Neal Cancer Center’s other shared facilities, has been used to develop a variety of new radioactive imaging agents that Yang suggests could light the way for the future of radiation therapy.
“If you take all the radiological and imaging studies that UAB has the ability to do, especially with the cyclotron, I think there have got to be ways that we can incorporate that technology and information to better deliver the radiation based on the biology of the cancer,” Yang said.
Part III: Chemotherapy
At the time of the dawn of the Cancer Center 50 years ago, researchers were still learning how cancer cells were different from the cells of normal, healthy tissue in the body. Because cancer cells inherently originate from within the body and because they divide quickly and at an unregulated, uncontrolled rate, it was demonstrably difficult to kill cancer cells or slow down their rate of division while leaving healthy cells unaffected.
Surgery, radiation and cytotoxic chemotherapy
In the early days of chemotherapy, the medications that were found to damage or slow the proliferation of cancer cells could not differentiate between the cancer and healthy cells in the body. The unintended damage to healthy cells and tissue as a result of these chemotherapy treatments led to a variety of the side effects observed.
While this kind of chemotherapy could inflict significant damage to tumor cells or reduce the spread of those tumor cells, the challenge for doctors and scientists was in developing new therapies that selectively damaged tumor cells without injuring healthy cells in the rest of the body.
Bassel El-Rayes, M.D., who recently joined the UAB O’Neal Comprehensive Cancer Center as its new deputy director, has spent his career working in translational cancer research to both improve treatments for patients and maintain their safety as those treatments are tested.
El-Rayes, who also serves as the director of the Division of Hematology & Oncology in the UAB Department of Medicine, explains that, because cancer cells divide much more quickly than other kinds of cells, early chemotherapies essentially functioned by impeding cell division in the body, regardless of whether the cells affected by the treatment were tumor cells or healthy cells.
“This type of chemotherapy is geared against the ability of cancer cells to divide, and they are using the fact that those cells divide constantly and in an unregulated way as their Achilles’ heel,” El-Rayes said.
“And even though it will have toxic effects on the other cells that normally divide in the body, the thought was that people will be able to recover,” added Barry Sleckman, M.D., Ph.D., director of the O’Neal Comprehensive Cancer Center. “And so what we have is a nonspecific therapy that is really targeted, not at the cancer, but at dividing cells, which is ineffective at treating the cancer in toxic to normal cells.”
For much of the history of cancer care in modern medicine, surgery and, later, radiation were considered the first line of defense in treating cancer, but like chemotherapy, both surgery and radiation could also cause unintended damage to healthy cells in the body.
“In the bigger scope of things, people used surgery to treat cancer long before they took radiation,” El-Rayes said. “Medications were really the new kids on the block.”
This first wave of chemotherapy medications, referred to as cytotoxic chemotherapy, worked by inhibiting the internal machinery upon which cancer cells depend to divide so quickly. And while this approach was effective in treating some cancers, it was not until researchers in the 1960s and 1970s began studying the relationships between genes, chromosomes, their mutations and alterations, and cellular biology in cancer that they were able to identify cancer-specific mutations, abnormalities and pathways that would allow chemotherapy medications to selectively target cancer cells.
Targeted chemotherapy
This opened the door for the second wave of chemotherapeutic medications in the advent of adjuvant chemotherapy, or targeted chemotherapy, which is a class of cancer drugs that target tumor cells based on their genetic abnormalities or on specific cellular pathways that are key to the survival and production of those cells.

Following the discovery of a chromosomal abnormality in the cancer cells of patients with chronic myelogenous leukemia in the 1960s and 1970s, researchers in the 1990s developed a new drug that would only affect cells with that specific abnormality, which was named Philadelphia chromosome translocation. According to the NCI, the discovery of the Philadelphia chromosome and the hybrid gene responsible for it, called BCR-ABL, demonstrated for the first time in history that a genetic alteration could cause cancer.
“And with that drug, we also noticed that the side effects were much lesser than the side effects of traditional cytotoxic chemotherapy,” El-Rayes said.
“So this drug, which specifically targets this kinase, can be used to treat CML patients orally. They just take a pill,” Sleckman added. “It doesn’t lead to any side effects – no hair loss, no GI toxicity, no bone marrow toxicity – but has a remarkable impact on the tumor cells.”
The drug, which was approved by the FDA in 2001, was called imatinib, or Gleevec, and worked by inhibiting a specific protein upon which the cancer cells in chronic myelogenous leukemia depended, functionally differentiating between the abnormal cancer cells, which overexpressed the gene that encoded this protein, and the normal, healthy cells, which were not so dependent on this protein for survival.
“The success of Gleevec was a proof of principle in that, if you had a cancer cell that is dependent on a protein and if you inhibited that protein, you could shut off that cancer cell,” El-Rayes said. “Gleevec is a turning point in cancer because it really demonstrated our ability to be selective. If you have the right drug and the right genetic alteration, you can achieve a lot without causing too much damage.”
The role of genetics
Genetic mutations and abnormalities can also be used to predict which patients will respond to specific kinds of treatments. For example, in 2004, researchers discovered that a lung cancer patient with a mutation that causes an epidermal growth factor receptor gene – a gene that builds receptors for a specific protein that stimulates growth in epidermal or epithelial cells – to remain active all the time was more likely to respond to a cancer treatment or medication that inhibits those growth factor receptors.

“At that point, the field moved because now it wasn’t just, ‘Let’s try the drug, see if it works or not and deal with the side effects,’” El-Rayes said. “Now, we had a way where we could select the patients who would respond to this drug and only treat those patients with it, which was the basis for personalized medicine in chemotherapy.”
This move away from what was once a one-size-fits-all approach to cancer treatment was also a move toward DNA testing, genomics and more targeted therapies.
“Not all cancers are the same,” El-Rayes said. “There are subgroups of these cancers that are addicted to different genetic alterations and that could be treated in different ways using these very selective drugs.”
Over the past decade or two, cancer researchers and doctors have been using genetics to predict patients’ risk of developing cancer, predict which patients will respond to certain treatments and predict patient outcomes, effectively using a patient’s individual genetic information to predict and manage that patient’s cancer, from prevention to prognosis to treatment.
“The introduction of targeted therapies and the understanding of the relationships between the cancer biology and, specifically, the driver mutations and the cancer cell addiction to these pathways opened the door for personalized medicine,” El-Rayes said. “The field has really grown since then, and it all started with being able to prove that certain genetic alterations or mutations can predict who will respond to certain drugs. That breakthrough meant that not only did we have targeted drugs, but now, we had a way to be personalized in our approach.”
Infusion in chemotherapy
In 2019, UAB opened the state of Alabama’s largest and only magnet-designated infusion therapy center. At this new, state-of-the-art clinic space in The Kirklin Clinic of UAB Hospital, patients with cancer and a variety of other conditions are treated with infusion therapy, which is a method of administering medication to a patient by inserting the medication directly into the patient’s vein.
This intravenous method of administering medication has proven useful for many patients in chemotherapy, as well as those receiving certain blood products, antibiotics, injections, central line care and immunotherapies. However, because an infusion therapy session can last up to several hours, UAB’s new, 84-chair infusion therapy clinic space was designed to give patients and their families more privacy and to make their experience more comfortable and convenient during their infusion therapy sessions.
In 2021, physicians from UAB Medicine, the UAB Heersink School of Medicine and the UAB O’Neal Comprehensive Cancer Center also launched a new Hepatic Artery Infusion Pump Program to offer more treatment options to patients with colon or rectal cancer that has spread to the liver. The HAIP Program is the only program of its type in Alabama and allows UAB to offer this high-dose chemotherapy infusion treatment to patients whose cancer has become inoperable.
Using this mechanism of chemotherapy treatment, surgeons insert an infusion pump roughly the size of a hockey puck underneath the patient’s skin and connect the pump to the patient’s hepatic artery using a small catheter. Administering chemotherapy through the infusion pump may help reduce the size and spread of a liver tumor, which could make surgical removal of the tumor more effective in the future, but if the liver tumor cannot be removed by surgery, the chemotherapy medications that are delivered by the infusion pump could still extend the lives of these cancer patients.
“I think that, as we advance, not only will there be new therapies, but there will be an emphasis on making sure that these treatments can be given in a way that is both comfortable and convenient for the patients and their families,” Sleckman said.
Immunochemotherapy
Regardless of how they are administered to the patient, cytotoxic chemotherapy and targeted chemotherapy do the same thing: use medications to fight cancer for the patient. However, in this new wave of chemotherapy treatments, immunochemotherapy uses medications to help the patient’s body fight the cancer using its own immune system.
“And with that, we saw some very remarkable responses. Unlike the responses that we had seen previously with chemotherapy and targeted drugs,” El-Rayes said, “with immunotherapy, we started to see much longer responses and much more sustained responses, which triggered a renewed excitement about this new class of agents and this new approach to the treatment of cancer.”
If a patient’s immune system no longer recognizes cancer cells as different from normal, healthy cells in the body, its immune response to those cancer cells has essentially been deactivated and will generally remain deactivated unless it recovers the ability to differentiate cancer cells from the rest of the body or unless it receives some kind of signal that prompts it to reactivate.
Immune checkpoint inhibitors are a class of medications that can both activate and deactivate an immune response. These drugs seek to help activate the body’s immune system so it will attack cancer cells, while also helping to deactivate the immune system so it does not attack healthy cells.
“It’s like the balance between your gas pedal and your brake pedal in the car,” El-Rayes said. “It’s the balance between those two that allows the car to travel at a certain speed, and it’s the balance between the stimulatory and inhibitory pathways in the immune system that allows your immune system to attack, for example, the bacteria and not attack the normal tissue.
“So, with the advent of immune checkpoint inhibitors, what we learned was that, if we loosen the brakes on the immune system, the immune system can come back and recognize the cancer again and attack it one more time.”
Part IV: Immunotherapy
Compared to other cancer treatment approaches, immunotherapy is the youngest, but interest in cancer immunology began long before it was even possible to identify the components of the immune system in a patient with cancer.

Until about 25 years ago, it was generally thought that there were no tumor-specific proteins or biomarkers that could be recognized by the body’s immune system, and if there were, the consensus was that the body’s immune system still had no effect on tumor cells.
It appeared to most researchers that the immune system was entirely incapable of differentiating between tumor cells and healthy cells, which both originate inside the body, in the same way that it was able to recognize viruses or bacteria. And at the time, there was no way to prove the existence of tumor-specific markers that were identifiable to the immune system, called tumor antigens, or to culture specific immune cells, such as T cells, in order to study them more closely.
Allan Zajac, Ph.D., is a senior scientist at the O’Neal Comprehensive Cancer Center and a professor in the UAB Department of Microbiology.
“In the 1990s, before I came to UAB, I met with a prominent cancer biologist who was very skeptical about tumor-associated antigens or tumor antigens, and his point was that you’re only going to see those in viral-induced tumors because it’s going to be a viral antigen,” Zajac said. “And over the next 20 years, I think we’ve seen that you do get neoantigens formed, you do get tumor antigens expressed, and you get cells of the immune system that respond to them.”
Zajac has spent the majority of his scientific career studying cell-mediated immune responses to viral infections, but his research on T cell responses, specifically T cell exhaustion, led him to apply his findings to the field of cancer immunology.
“A lot of the discoveries that we’ve made using viral model systems have become generally applicable, whether it’s to a tumor system or whether it’s to other viral infections or other conditions as well,” Zajac said. “And I would say that the findings that we’ve made in viral systems have probably made more of an impact on cancers than they have on infections because the understanding of the exhausted subsets and use of checkpoint blockade inhibitors to try and rejuvenate responses has been shown to be really beneficial for cancer treatments.”
Genetic abnormalities and checkpoint inhibitors
Scientists learned that, at least in some cancers, T cells were recognizing and responding to tumor cells, suggesting the presence of a tumor antigen that the body’s immune system could “see” and identify as different from itself. But why was this immune response possible or more likely for certain types of cancer than others?

Frances Lund, Ph.D., a senior scientist at the O’Neal Cancer Center and the director of the UAB Immunology Institute, suggests that one explanation developed as researchers observed that the mutation load for some cancers was higher than it was in others, meaning that the tumor cells of some cancers were undergoing more genetic mutations than the tumor cells present in other kinds of cancer.
“We finally came to the understanding that, for certain kinds of cancer, for whatever reason, the cancer cells undergo many, many more rounds of changes in their genome that result in modifications of the proteins that normally your body would consider ‘self,'” Lund said. “But now, the cancer cells look different, and so now, the immune system can actually see it. And that took a long time to understand.”
The immune system cannot always “see” tumor cells the way it can cells that are foreign to the body, such as viruses and bacteria, but the more a tumor cell mutates, the more likely it is to produce new antigens that the immune system can “see” and, therefore, attack.
This explains why patients with some cancers – particularly, those with a higher mutation load – often had a better response to immune checkpoint inhibitors, which essentially loosened the brakes on an immune system that had already identified tumor cells as its target. Cutting the brakes on the immune system worked best when the immune system knew what it was supposed to be fighting.
The brakes themselves are thought to normally function by deactivating T cells before they cause too much damage to healthy cells, so the body can begin to repair some of that damage. But when checkpoint inhibitors block the T cells’ ability to deactivate, it can trigger a full-blown immune response that can result in serious inflammatory conditions for patients.
Lund and her husband, Troy Randall, Ph.D., who is also a senior scientist in the O’Neal Cancer Center, share a research laboratory at UAB that studies the biological mechanisms that control protective immunity to pathogens and how cancer and other chronic infectious, allergic autoimmune diseases subvert those mechanisms.
“All immunotherapy comes with risk of inflammatory side effects,” Lund said. “We are learning more about which immunotherapies, whether given alone or in combination, are effective in promoting anti-tumor immunity, while at the same time, causing the least serious side effects.”
Randall is a professor of Clinical Immunology & Rheumatology in the UAB Department of Medicine and also serves as a co-leader of the O’Neal Cancer Center’s Cancer Biology & Immunology Research Program.
“At the beginning of immunology, even for the first hundred years of it, what everybody was focused on was how do you get an immune response started, like to a vaccine or to an infection or something like that, and how does it work to kill the infection?” Randall said. “And then suddenly, about 25 to 30 years ago, people started to realize that there’s just as many things that turn the immune system off as there are that turn it on.
“And so, part of the dance that we have to play is that we need to reactivate the immune system in tumors, and we need to deactivate these repressive mechanisms.”
T cell exhaustion, imaging and genomic sequencing
When T cells do recognize a persistent antigen – often seen in long-term viral infections or, more recently, cancer – those T cells can also eventually become exhausted, making it more difficult for them to reactivate when they encounter a tumor cell. But checkpoint blockade therapies can help them recharge and reactivate.

Zajac’s primary area of expertise lies in T cell exhaustion, which is common in cancer and a variety of other chronic conditions.
“In infections, such as HIV or hepatitis C or tumors, which you never get rid of, the T cells have to adapt to those conditions and can actually start to turn off their responsiveness,” he said. “And in the context of an infection, which is what our immune system has evolved to fight, that’s probably really important to limit damage caused by the T cell.”
However, as researchers developed new antibodies that could bind to specific proteins attached to immune cells and, later, specific proteins attached to tumor cells, they were able to use techniques such as flow cytometry and major histocompatibility complex tetramers to detect and observe those cells.
These advances in technology allowed researchers to see that immune cells were physically present in a tumor, even if they weren’t functioning, as was the case for T cell exhaustion.
“So it’s like going into a room and being able to count people: You know they’re there, but you don’t know what they do,” Zajac said. “In this case, when it was first discovered that they were present, we knew that the T cells could recognize the virus, but we couldn’t measure any functional activities.
“The use of MHC tetramers and better single-cell analysis has allowed us to scrutinize tumor-infiltrating populations and tumor-specific populations to a level that was just unheard of a couple of decades ago.”
Lund explains that these advancements in imaging enabled scientists to categorize tumors according to the presence and quantity of T cells in or around tumor cells, even if those T cells were not fighting the tumor.
“We can now define tumors in two ways: We can define them by their mutation load and whether they are surrounded by T cells – which is what we call a ‘hot’ tumor – or don’t have immune cells around them – which is what we call a ‘cold’ tumor,” Lund said. “If we can use immunotherapy to take away the exhausted phenotype of the cancer T cells that are near the tumor cells in a hot tumor and if the tumor has a high mutation load and presents plenty of things for the immune system to see, then immunotherapy can help a lot.”
The 1990s also saw the rise of genomic sequencing, which revolutionized the field by finally giving scientists the ability to see different genetic mutations, some of which were later identified as tumor antigens.
“I think the secret is in technology, because now you could identify potential changes in the tumors that allowed them to express particular tumor antigens,” Zajac said. “So these sequencing technologies and some proteomic technologies have really helped reveal the presence of the antigens.”
Randall says the O’Neal Cancer Center helped kick off the “big sequencing revolution” back in 1987 when it purchased one of the nation’s first DNA sequencers. At the time, the Cancer Center was able to obtain this cutting-edge equipment with the assistance of the Cancer Center Supporters Board, now named the Advisory Board of the O’Neal Comprehensive Cancer Center, which successfully raised the funds necessary to purchase the sequencer.
“The ability to figure out what’s in a tumor and what those cells are and what they do, including the tumor cells themselves, is just exponentially more now than we could’ve ever done before,” Randall said.
Tumor antigens and targeted checkpoint therapies
The greatest breakthrough in cancer immunotherapy came with the long-awaited discovery of two specific molecules – CTLA-4 and PD-1 – that were thought to be the proteins responsible for T cell deactivation and exhaustion. Soon, researchers were able to develop antibodies that could bind to those two molecules, making the tumor cell visible to the immune system, and that could inhibit the ability of CTLA-4 and PD-1 to shut down the immune response of nearby T cells.
Once researchers found that the CTLA-4 and PD-1 molecules were becoming upregulated on the unresponsive T cells, they learned they could block the interaction inhibiting the T cells’ response by introducing anti-CTLA-4 and anti-PD-1 antibodies that could prevent those molecules from operating.
“And that really helped cement the notion that the T cells were being actively downregulated, and if you could block these inhibitory interactions using checkpoint blockade therapies, you may be able to rejuvenate those cells and get them to do something useful in terms of viral control, or especially in terms of tumor control,” Zajac said.
This discovery demonstrated that not only were tumor antigens present, but they were the product of now-identifiable genetic mutations that served the tumor cell by functionally slamming on the brakes of the body’s immune system. By cutting the brakes on that immune system and putting it on a track headed straight for those tumor antigens, the immune system could finally begin to take down tumor cells.
Since then, researchers have developed more checkpoint inhibitors like anti-CTLA-4 and anti-PD-1 for a variety of other cancers and can use technologies such as genetic sequencing, flow cytometry and proteomics to predict which patients will benefit from those therapies.
“It’s really only in the last 15 to 20 years that we’ve been able to see the cells in the tumor and really understand what’s there, what their phenotype is and what it is that they might be able to do functionally,” Lund said. “And before, we couldn’t do any of that.”
“So part of that’s related to sequencing, and part of it’s related to the flow cytometry technology. Now there’s PET imaging and MRI imaging, and the resolution on those is way better than it ever used to be,” Randall added. “So all of that combined just gives us so much more information about what’s going on, or in some cases, what’s not going on – like if the immune system is not working in a particular tumor – that really informs how we would treat patients.”
Combination immunotherapies
In the beginning, immunotherapy was still experimental and so was reserved for cancer patients who had already gone through the gamut of other treatments, such as radiation therapy, chemotherapy or surgery, to little avail. But because those treatments could also take a toll on the body’s immune system, patients did not have much of an immune system left for the immune therapies to work with by the time they were receiving those therapies.
“So if you get the immunotherapy treatment earlier, that’s at a time when maybe we can actually recover your immune system a little bit more,” Lund said. “If we wait until you’ve failed everything else, it may not be possible to turn it around at that point.”
But as the field progressed, especially over the past decade, doctors and researchers found that combining immunotherapy with other treatments that served to damage tumor cells also caused the tumor cells to produce more antigens that were visible to the immune system and increased the effects of immune therapy.
“If you come in with chemotherapy or radiation, what that does is it damages the tumor, and it releases things from the tumor that the immune system can now see,” Lund said. “And so, even if the T cells are normally excluded from getting in the tumor, if you put a big hole in the middle of it and let everything out, then maybe the T cells can get there, or at least get activated.”
At the O’Neal Cancer Center, specialists in chemotherapy, radiation therapy, surgical oncology, immunotherapy and a variety of other disciplines work closely together to develop individual treatment plans for patients.
“So the idea is that you take the brakes off and give the immune system something to see, and the way that you give it something to see is you give the patients chemo or radiation, and then you give them immunotherapy,” Lund said.
Immunotherapies are not an all-purpose cure for everyone’s cancer, but Lund and Randall say the future of the field is in learning why certain treatments are effective for only some patients and how the immune system could be used to fight cancer in new ways.
“So some of that is really trying to understand how does a drug change the immune system in some people and not in others,” Lund said. “And what’s in development right now are other kinds of therapies that would activate other arms of the immune system that might also help to eliminate tumors.”
Randall says the field has come a long way, both in general and at UAB. Through the O’Neal Cancer Service Line, the operational arm of clinical care delivery at the O’Neal Cancer Center, these cancer therapies are now carefully selected and planned for each patient, depending on the patient’s cancer, genetic information and other factors.
“We realize now that there are literally hundreds more of these mechanisms that are shutting down the immune response,” Randall said. “And so we’re trying to learn which mechanisms are being used in which tumors and how do we intervene to overcome that –“
“– and how do we intervene in a way that we don’t cause the immune system to go awry,” Lund added.
Epilogue: Faith in the future
In the decades since the word was considered unmentionable, since treatments were broadly thought of as futile and since some methods of screening were just as stigmatized as the disease itself, cancer has come a long way in little more than a half-century.
As former NCI Assistant Director Otis Brawley, M.D., explained to U.S. News & World Report in 2018, some cancer screenings – such as pap smears to detect cervical cancer – were uncomfortable to discuss, much less undergo, prior to the 1960s. But when President Richard Nixon signed the National Cancer Act of 1971 and the nation began to invest more resources in the study and treatment of cancer, it “really started putting momentum into cancer, and people started saying it more and more,” Brawley said.
This robust federal commitment to cancer research that created the UAB O’Neal Comprehensive Cancer Center was, at least in part, powered by a renewed public zeal for studying, treating and diagnosing cancer, similar to the grassroots movement in Alabama to build the state’s first cancer research hospital back in the 1960s and 1970s.
“When I started at the Cancer Center in September 1969, usually if surgery and radiation didn’t take care of a patient’s cancer, they used chemotherapy as a last resort,” Kemp said. “We had four drugs that I can remember, and that was kind of it.”
The development of more effective treatments and tests for cancer over the past 50 years has paved the way for a paradigm shift in cancer medicine and academic research, which has also led to the evolution of many medical specialties dedicated to cancer, some of which we now know as surgical oncology, radiation oncology, medical oncology and cancer immunology.
“I think the outlook on cancer treatments, because we have so many better drugs and different treatment modalities – the radiation therapy, the proton therapy, all the surgical techniques now with robotics – there’s just really no comparison from the way it is now to the way it was then,” Kemp said.
As these developments and associated concepts in cancer control, such as early detection and prevention, have become more understood and normalized among patients, their families, providers, scientists, medical leaders and the public at large, cancer as a condition – as well as, consequently, the word “cancer” itself – seems to have shed some of the cultural stigma that previously shrouded the disease and many of the treatments and screenings for it.
“From that point to where they are today, 50 years later, with personalized medicine, targeted treatments and other targeted modalities, it really is amazing,” Kemp said.




